MANAGEMENT of tos
Treatment of TOS is dependent on the type of symptoms that the patient is presenting with. nTOS is generally managed with conservative treatment, whereas vTOS and aTOS require surgical intervention (Jones et al., 2019). Pharmacological treatments offer temporary relief from symptoms, including nonsteroidal anti-inflammatories (NSAIDs), anticonvulsants and muscle relaxants (Brooke & Freischlag, 2010). Experimental interventions have also been depicted in literature with including steroid injection, Botulinum toxin A, or local anaesthetic into the pectoralis minor and scalene muscles which have had varying success in observational studies (Foley et al., 2012).
Physiotherapy is a widely recommended treatment for nTOS and must entail education surrounding weight control, and ergonomics at work and home to maintain adequate postures (Jones et al., 2019). Physiotherapy interventions should also incorporate activity modifications, as well as stretching and strengthening the active muscles of the neck, chest, and upper arm to release pressure on the thoracic outlet (Huang & Zager, 2004).
Physiotherapy for NTOS
Initial treatment should revolve around pain relief and postural correction with frequent sessions (2-3 x per week). Once pain is well managed, treatment should progress to muscle stretching and strengthening. Throughout this period, treatment sessions should decrease (1x per week), although the patient should be completing a home exercise program (HEP). The total physiotherapy recovery period generally consists of 8-12 weeks, however, this is extremely variable between specific patient cases (Camporese et al., 2022).
Heat or ice may be applied to the neck and shoulder to decrease muscle tightness and inflammation. Manual therapy, neural glides, and postural correction interventions should also be incorporated into treatment to reduce nerve irritation and alleviate symptoms (Luu et al., 2022).
POSTURAL CORRECTION
During the initial phase of treatment, it is essential to address poor postural habits. Correcting forward head posture and thoracic kyphosis is conducted by instructing patients to align their ears over their shoulders. Avoiding slouching while seated is also extremely important in this stage and may be corrected by cueing the patient to imagine a rod in their back, to maintain a neutral spine (Larsen, 2018). Furthermore, implementing ergonomic modifications is necessary to reduce nerve irritation. Adjust the chair and desk height at work and at home to ensure the feet are flat on the floor and the forearms are parallel to the ground when typing. Ensure the keyboard and mouse are close to the patient to reduce excessive reaching. Encourage frequent breaks every 30-60 minutes (Larsen, 2018).
In clinic, it is essential to reset the scapula to promote a neutral position without over-elevating or depressing. Scapula resetting generally consists of small isometric contractions with the patient using their fingers to feel the contraction of the muscles around the scapula.
MANUAL THERAPY
Techniques such as myofascial release, trigger point therapy, and deep tissue massage should be used to reduce muscle tightness in the scalene, pectoralis minor, and subclavius muscles surrounding the thoracic outlet, to alleviate compression on the brachial plexus (Watson et al., 2010).
First rib mobilisations may be incorporated into treatment as the top of the ribcage beneath the clavicle may become stiff, thus, causing brachial plexus compression. The patient lies supine and the therapist palpates the first rib. The physio then applies a downward and medial force towards the opposite hip using small oscillations (Boehm, 2013).
The thoracic spine may also become stiff due to TOS, restricting shoulder, rib, and neck movements. The thoracic spine is mobilised with the patient in a prone position, as the therapist palpates the thoracic vertebrae. The mobilisations are generally conducted in a posterior to anterior direction on the spinous transverse processes. If the patient reports pain a Grade I or II mobilisation may be utilised, however, if they only report stiffness, Grade III or IV oscillations may be applied (Boehm, 2013).
Frequency: 5-10 minutes per session
Intensity: Light pressure with patient feedback to not invoke pain
Type: Begin with effleurage massage and progress to deep tissue techniques and trigger point therapy.
NEURAL GLIDES
Neural glides can restore brachial plexus mobility and reduce neural tension in the thoracic outlet. However, they may invoke symptoms of pain, so it is imperative to allow patient feedback to guide treatment (Luu et al., 2022).
Median nerve glide: Extend and abduct the arm with the palm supinated, extend the wrist, rotate the shoulder externally and slowly tilt the head away from the affected arm to tension the nerve. To perform the glide, move the wrist and hand to neutral and the head to its normal resting position (Luu et al., 2022).
Ulnar Nerve Glide: Abduct the shoulder, flex the elbow, extend the wrist, and tilt the neck away. Move the wrist and hand to neutral and rest the head to perform a gliding movement (Luu et al., 2022).
Nerve glides must only be utilised for the appropriate patients, as they can cause excessive irritation and shearing of the nerves leading to increased pain and discomfort.
Frequency: Daily
Time: 10-15 repetitions 1 set
TAPING FOR TOS
Studies have depicted that taping is effective in the management of TOS as it addresses the biomechanical and neurological factors that cause the condition. Axillary taping has been found to provide scapula alignment and enhance stability whilst reducing parasthesia and pain. Furthermore, taping improves upper limb function by supporting the weak muscles and inhibiting the hypertonic muscles to balance the muscular forces in the thoracic outlet for patients with symptomatic TOS (Ortac et al., 2020).
Stretching and Strengthening Exercises
Stretching exercises should target the muscles surrounding the thoracic outlet, including the scalene muscles, levator scapulae, pectoralis minor, subclavius, and upper trapezius muscles. Thoracic extensions with a foam roller under the mid-spine should also be included (Lo et al., 2011).
Frequency: Daily
Intensity: Moderate
Time: 10 repetitions 1 set, 15-20 second holds
Strengthening exercises should incorporate resisted cranio-cervical flexor and extensor training, prone Y, T, W and L raises, resistance band rows, serratus anterior punch, and resistance band shoulder external and internal rotation exercises. These exercises are conveyed in the physiotherapy session and incorporated into the HEP (Lo et al., 2011).
These exercises aim to strengthen the muscles around the thoracic outlet, so they are activated in symmetry to assist the upward rotation of the scapula (Watson et al., 2010).
Frequency: 2-3 x per week
Intensity: Moderate resistance
Time: 10-15 repetitions
Activity Modifications
Modifying sports mechanics to reduce the repetition of overhead movements, to remove extensive pressure on the shoulder girdle. The focus for athletes should be to strengthen the shoulder. Alter repetitive tasks in the patient’s daily life to avoid prolonged static postures. Ensure patients involved in heavy lifting are bending at the knees, keeping objects close to the body, and seeking assistance if needed (Hooper et al., 2010).
Different positioning cues depend on the current scapula position the patient presents with (Watson et al., 2010).
A: Scapula depression
B: Posterior tilt of the scapula
C: Medial glide of the scapula
Axillary taping holds the scapula in an upward rotation and elevated position to reduce tension on the thoracic outlet
(Watson et al., 2010).
(Precision movement, 2023)
Levator scapulae stretch
Serratus anterior punches with dumbbell - improves scapula positioning and stability reducing tension at the brachial plexus (Jones et al., 2019).
(Muscolino, 2020)
Upper trapezius stretch
Prone Y, T, W and L raises - improve scapular control and motion for patients with TOS (Lo et al., 2011)
(George, 2023).
(Kasparson, 2016)
Surgical intervention
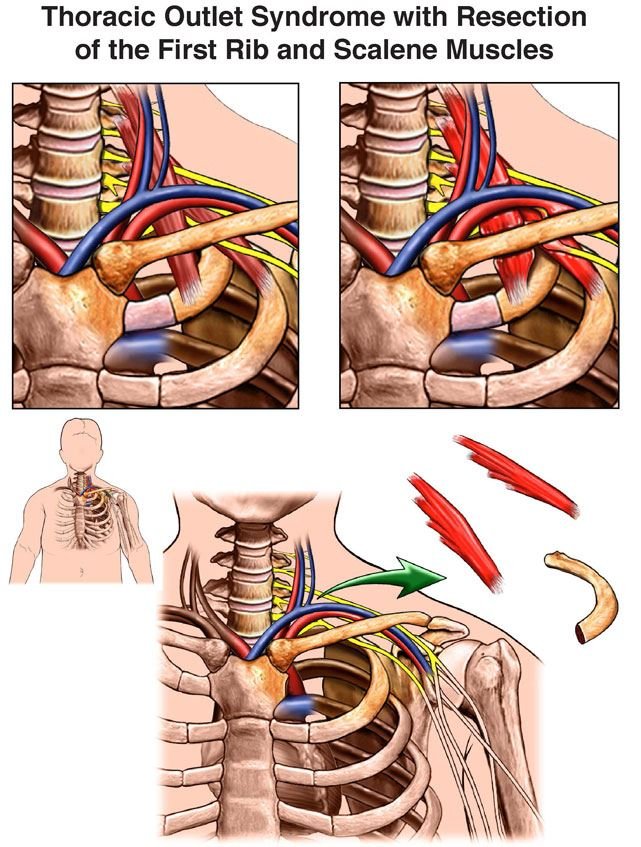
Surgery is the recommended intervention vTOS and aTOS immediately following diagnosis due to the life-threatening effects of thrombosis and ischemia, and the inability to treat in clinical practice (Burt, 2018). However, surgery may also be considered for nTOS if conservative management is ineffective over a 3-4 month period. The most common surgical procedure is a first rib resection to decrease compression at the brachial plexus (Jones et al., 2019).
Three separate surgical approaches reduce brachial plexus compression, they include infraclavicular, transaxillary, and supraclavicular techniques (Peek et al., 2017).
The infraclavicular approach is the least frequent of the three, and it entails an incision below the collarbone to access the subclavian vein, and pectoralis minor muscles to reduce compression for patients with vTOS. The supraclavicular approach involves an incision above the collarbone to target the brachial plexus and a scalenectomy of the anterior and middle scalene muscles to access the first rib. The transaxillary technique refers to an incision made between the pectoralis major and latissimus dorsi muscles in the axilla, allowing access to resect the first rib and reduce compression at the brachial plexus and subclavian vein (Chang et al., 2009).
Other surgeries consist of a clavicle resection to increase space in the thoracic outlet and a pectoralis minor tenotomy which is conducted to release pressure in the brachial plexus as it passes under the pectoralis minor muscle (Huang & Zager, 2009).
Physiotherapy post-surgery follows the same guidelines as the aforementioned interventions, focussing on postural correction, stretching and strengthening the muscles surrounding the thoracic outlet (Jones et al., 2019).
(HeafnerHealth, 2022)
(Burt, 2018).